Industry Update, November 2023

Hi Everyone,
Now we are a full year into working with our funding tool, the Department of Health are undertaking series of analysis to determine if any changes are needed to the model, the class’s, the NWAU and approach to the price point.
No doubt there will be advice provided prior to the Christmas break so please ensure you keep an eye out on any communications and webinars.
aged care funding reform committee
Our November meeting kicked off with discussions on analysis received by Stewart Brown on the significant changes this last financial year with agency use to supplicate the compliance with RN 24/7 legislation. Discussions by committee members acknowledged the difficulty most providers have with affording agency, recruiting and retaining staff, and remaining financially sustainable with the new legislations and compliances.
Deliberations were undertaken if there really was a significant workforce shortage, or if the workforce was available, just moved across to agencies for higher wages, improved choices around working conditions and how people choose to work. Also considered was the higher cost of living and affordability of accommodation influencing particularly rural and remote regions, both which further impact the financial outcomes when you consider travel costs and accommodation costs applied on top of the agency charges.
Note – our industry has a capital assistance program available to support the costs of accommodation for health staff
https://www.health.gov.au/our-work/aged-care-capital-assistance-program
Details from Stewart Brown follows
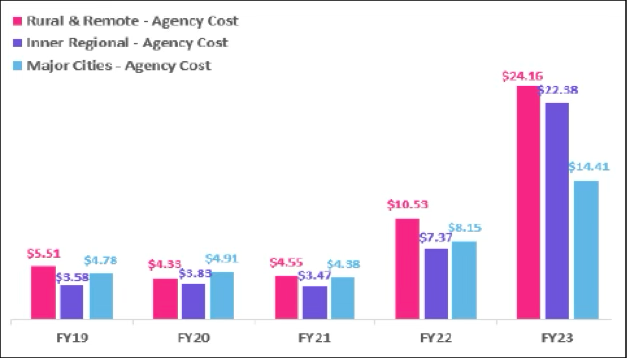
StewartBrown have reported in their Aged Care Financial Performance Survey Report for 2022-23 that agency costs for direct care (inclusive of RNs, enrolled nurses and personal care workers) have increased significantly from the previous financial year:
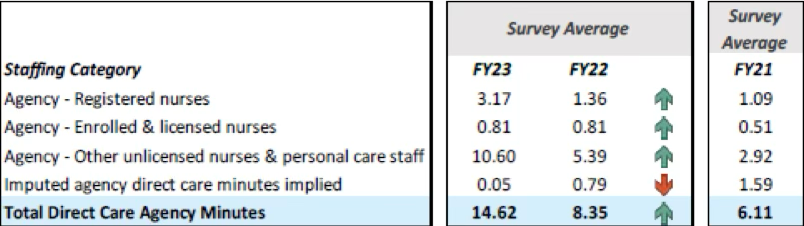
The StewartBrown report also highlights that agency minutes has also seen an increase from the previous financial year:
QFR Analysis
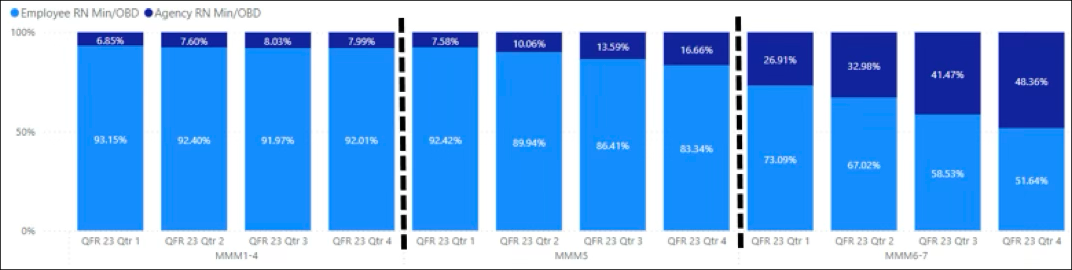
- The QFR shows that across the reporting quarters there is some increase in the use of agency RN minutes in MMM5 and a significant increase in MMM6-7.
|
|
QFR 23 Qtr 1 |
QFR 23 Qtr 2 |
QFR 23 Qtr 3 |
QFR 23 Qtr 4 |
||||||||
|
|
RN Target |
Direct |
Agency |
RN Target |
Direct |
Agency |
RN Target |
Direct |
Agency |
RN Target |
Direct |
Agency |
|
MMM1-4 |
39.56 |
31.18 |
2.29 |
39.46 |
31.42 |
2.58 |
39.52 |
31.96 |
2.79 |
39.70 |
33.51 |
2.91 |
|
MMM5 |
39.29 |
34.99 |
2.87 |
39.12 |
35.87 |
4.01 |
39.10 |
34.99 |
5.50 |
39.20 |
34.65 |
6.93 |
|
MMM6-7 |
39.24 |
29.92 |
11.02 |
38.14 |
29.29 |
14.41 |
37.95 |
29.56 |
20.95 |
38.17 |
25.69 |
24.06 |
- Whilst the usage of agency RNs in MMM1-4 is steady and less than 10% of RN minutes across the quarters, the agency staff cost per hour is between 46 and 57% more than direct employed. The costs for agency staff in MMM6-7 is around 80% more than direct employed, this could be attributed to fly-in/fly-out costs.
|
|
QFR 23 Qtr 1 |
QFR 23 Qtr 2 |
QFR 23 Qtr 3 |
QFR 23 Qtr 4 |
||||
|
|
Employee |
Agency |
Employee |
Agency |
Employee |
Agency |
Employee |
Agency |
|
MMM1-4 |
$67.85 |
$99.79 |
$69.91 |
$102.40 |
$70.74 |
$110.90 |
$73.57 |
$112.14 |
|
MMM5 |
$68.95 |
$113.56 |
$68.33 |
$116.08 |
$69.02 |
$115.48 |
$72.08 |
$120.82 |
|
MMM6-7 |
$72.51 |
$143.52 |
$67.23 |
$124.00 |
$71.93 |
$129.79 |
$72.50 |
$128.86 |
Following on we discussed how the government could support providers to incentivize attraction and retention of permanent staff to minimize this trend of higher agency use. A number of options were tabled, most of the committee members agreed any kind of incentivized support needed to be well considered to prevent perverse or unintended consequences. Further information to determine longer term trends are to be considered before progressing with any actions in this area.
Palliative Care
As you would have noted from my earlier emails, the palliative care process for Class 1 has changed allowing for an extra 14 days post admission to complete the palliative care status form. Further changes are expected with additional evidence to be added to this process preventing manipulation of the rules.
The DoH explained one provider who shall remain nameless, has been discharging residents then admitting again the next day to qualify for a class 1. Inventive I have to say.
Further available supplements for end of life is being strongly considered, the committee agreed on a process with acceptable and reasonable guidelines to support the costs of end of life care in the last 7 days. It is likely the process will be similar to the palliative care status form with some changes in the Karnovsky for example. Payments will be per day and only paid for 7 days.
Alternative Arrangements
Tenders are being sought for the design of a study to take place in specialized services such as homeless or ATSI to determine if additional care minutes and funding is needed to support the additional care needs of specialized groups. The previous study now completed by the University of Wollongong is undecided in their conclusion which has led to a continuation of further research. It is planned a framework and model of funding and care will then be applied.
RN 24/7 and Care Minute audits
Our feedback has been heard and acted upon fairly quickly I must say, on the amount of detail and work required to complete the evidence requested for the RN 24/7 and care minute remote audits by the DoH.
Further discussion will be had when we resume in the new year, however we received assurance the process of uploading data will be simplified prior to the end of November, likely to be similar to ACFI evidence uploading processes.
Consideration on the information requested and ability to reduce and streamline data collection is being analysed as we speak.
Your contributions and feedback do result in actions so well done!.
Whilst on the topic, did you know that any overtime a Facility Manager or Care Manager may undertake (if they are a RN), counts to additional RN care minutes – see feedback below
As per the Quarterly Financial Report (QFR) definitions, for the purposes of care minutes reporting only time providing direct care activities by a registered nurse on-site (including one-on-one and non-face-to-face care) can count towards a RN's direct care hours. Activities considered to count as direct care for the purposes of care minutes are outlined in table 1 in section 3.1 of the Care minutes and 24/7 registered nurse responsibility guide.
• Where an RN is employed in a hybrid role, for example as a Facility Manager providing both direct care and other activities such as care management only the portion of the worker’s time spent on direct care can count towards RN labour costs.
• Support provided through on-call/ weekend phone calls and virtual telehealth arrangements cannot contribute towards RN care minutes.
• As above, only the portion of overtime hours providing direct care activities by a registered nurse on-site can be counted towards RN care minutes.
For further information about care minutes reporting, please see the Care minutes and 24/7 registered nurse responsibility guide on the Department of Health and Aged Care website.
Also, a reminder that emotional support provided to the resident AND their family counts to care


